You would think that in view of the large number of procedures undertaken in the NHS that the science would be driving the procedure, when in fact it is more custom and practise tinged heavily with vested interests and hubris. Orthopods (Orthopaedic Surgeon's) are generally viewed by Medicine, even other Surgeons as lacking in subtlety and intelligence. My view is somewhat more colourful and I view them as 'butchers' more than surgeons. Sure, it's a hard job, requiring physical strength and endurance, almost as much as skill because of the need to saw, hammer, drill and slice, with instruments more akin to a construction site and a butchers shop than an operating theatre. And the repair (or often not) of damaged hips epitomises this more than any other procedure. Dealing with hip trauma is probably the most difficult and dangerous procedure any surgeon undertakes. It is important then that the patient is paramount in the evaluation of which path to pursue as regards the protocol that is most efficacious.
It is not beyond my purview that many 'orthopods' are failed Rugby players, not that I attach any significance to that, except to say that their adherence to scientific evidence as a tenet of their professional conduct is perhaps somewhat lacking. It may sometimes be evident that their judgement of certain medical devices might be coloured by the presentation they last 'endured' in Barbados about the latest implantable device from one of the many makers of such engineering masterpieces (sic). One of these, of course is Depuy, a subsidiary of Johnson and Johnson (a family company). They make the 'Pinnacle' implant, which is a MOM (metal on metal) device using cobalt chrome, and this has been indicted as being subject to early failure. And more importantly, (I feel) of causing the migration into the bloodstream, bone and other tissues, of wear particles that are potentially life threatening in a number of ways.
The BMJ in conjunction with Newsnight undertook a study recently that highlighted this problem that is faced by a number of 'younger' patients who have been ill served by the installation of this design of prosthesis into their acetabulum. In truth the BMJ article is somewhat more comprehensive in it's condemnation of the device than was Paxman in the interview with the head 'honcho' of the MHRA who, it would seem had full knowledge of the 2010 recall by Depuy of it's ASR implant (Pinnacle) but seems to have done little about it. Nonetheless I did enjoy Paxman's taking Kent Wood's to task about the fundamentally supine attitude of his organisation when it comes to 'approving' medical devices, which essentially amounts to a review of the specification provided by the makers, because there are few if any clinical trials undertaken, except using the patient cohort as 'guinea pigs'.
As an engineer first and biologist second (but linking the two), I cannot understand how anyone would recommend the installation of any ball and socket device, in the human made from cobalt chrome that will be subject to metal on metal wear or indeed any frictional wear. The cobalt element of the material does have high strength, coupled with excellent corrosion resistance, but whilst it's salts are used by most animals especially ruminants, at high levels it can be toxic and it's compounds have been responsible for cardiomyopathy (heart muscle disease) in humans. Chromium is also quite toxic in its (VI) form except at very low levels and is a known carcinogen as well as being responsible for damage to the kidneys, liver and blood cells. Having said that, if this material had only been utilised for non-frictional component parts it is unlikely that there would have been a problem, but friction in metal to metal bearings throws off metal ions, eroding interfaces which increases gaps in mating surfaces thus introducing 'free play'. This is of course exponential, so the more wear the more the acceleration of that wear. The consequent contamination of the tissue surrounding the acetabulum and femoral stem and migration of these metal ions into the bloodstream promotes high levels of bone loss, cement collar erosion, cartilage damage, and many other toxic side effects that have yet to be fully evaluated.
When you introduce any 'foreign' body or substance into any living organism you have to be very sure that by so doing you are not making matters worse, but obviously this did not seem to impinge upon the corporate 'psyche' of J and J. Greed seems to have been the driving force and don't forget this company had last quarter earnings of $16.3 billion despite having to pay out $3 billion for the Pinnacle debacle in the US.
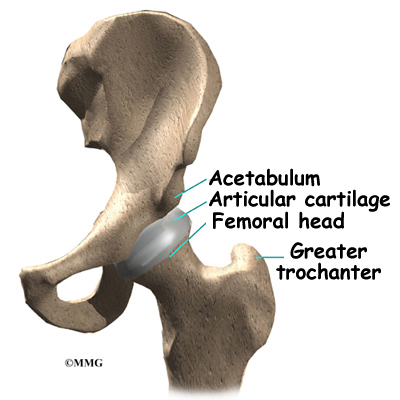 This design of implant was targeted at the younger audience and was sold as a 'low wear' prosthetic so as to avoid the need for revision surgery because this cohort tends to be physically very active. Activity promotes wear in any joint be it in humans' or in machinery, unless you can regularly lubricate that joint. There is some value in the concept of synovial fluid performing this function (the hip joints natural lubricant and hydraulic 'cushion'), but as this 'capsule' has effectively to be 'burst' during surgery for access, it is unlikely to function as it was designed by nature thereafter. The simple truth is that in our haste to address the increasing needs of an ageing and increasingly joint challenged society we have lost sight of many of the needs attendant upon the production of manufactured joints for implanting. And sadly it is not just in the metal to metal prosthetics that we have a problem.Many different materials have been tried over the years, especially plastics, sintered metals and ceramics. If one views success as being a bearing surface that does not wear out at all, and what wear does take place as being entirely benign, manufacturers have failed. Failed miserably in this context because all arthroplasty components have a finite life, so except in elderly patients, they are unlikely not to need revision at least once and in young patients possibly more.
This design of implant was targeted at the younger audience and was sold as a 'low wear' prosthetic so as to avoid the need for revision surgery because this cohort tends to be physically very active. Activity promotes wear in any joint be it in humans' or in machinery, unless you can regularly lubricate that joint. There is some value in the concept of synovial fluid performing this function (the hip joints natural lubricant and hydraulic 'cushion'), but as this 'capsule' has effectively to be 'burst' during surgery for access, it is unlikely to function as it was designed by nature thereafter. The simple truth is that in our haste to address the increasing needs of an ageing and increasingly joint challenged society we have lost sight of many of the needs attendant upon the production of manufactured joints for implanting. And sadly it is not just in the metal to metal prosthetics that we have a problem.Many different materials have been tried over the years, especially plastics, sintered metals and ceramics. If one views success as being a bearing surface that does not wear out at all, and what wear does take place as being entirely benign, manufacturers have failed. Failed miserably in this context because all arthroplasty components have a finite life, so except in elderly patients, they are unlikely not to need revision at least once and in young patients possibly more.UHMWPE has been the material of choice especially the newer 'crosslinked' varieties, for the manufacture of joint surfaces for some years now. Ultra high molecular weight polyethylene displays admirable self lubricating properties together little moisture absorption and considerable strength. But combinations of both this, ceramics and other metals have been tried, to come up with this goal of the perfect implant. None, including UHMWPE is devoid of particulate contamination of the tissue and blood of the recipient, although this last one is probably more benign than others. None are entirely so, and all wear is at a rate in proportion to the amount of use. So active people wear their implants out quicker.
As regards the NHS; well they invariably go for the cheapest they can get away with, THA (total hip arthroplasty) using cemented stems and UHMWPE bearing surfaces is usually the type most will get for either trauma repair or elective surgery, generally for osteoarthritis of the hip. Except for non-displaced or slightly displaced fractures, when the waters become extremely muddied. This is because of the payment system that prevails in trauma care which is based on a tariff for the most expensive treatment involved in a hospital 'stay', and the desire to keep the costs low, avoid re-admission and get rid of you as soon as possible. Trauma patients 'bugger up' the system, take up unplanned beds and play havoc with operating lists and theatre time allocations. If you aren't fixed quickly it costs more than the tariff. If they do something that's possibly short term, even if it's in your best interest as a patient, it's likely not to happen. If you are re-admitted for something that's a result of your initial admission, they won't get paid for it, so you are a burden.
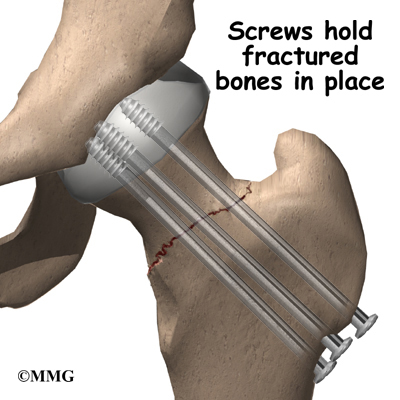 This has resulted on many occasions in the almost complete lack of hip repairs in trauma patients because of the incidence of failure. This is despite the fact that preservation of the native acetabulum and femoral head is the ideal solution. Failure rates of hip repairs are the subject of much conjecture but they are only about 25% in reasonably healthy people up to 65 or 70 years. They are also quick to do, much less traumatic, and can be undertaken, often without general anaesthetic, and sometimes without incision. Generally this requires nails or screws to fasten the joint together which are then left in place. If this fails, then you can go on to have a full procedure at a more leisurely pace and not as an emergency. But it won't happen, because if it fails, the Hospital involved will not get paid for the subsequent and much more expensive procedure to fix it because the 'system' attributes the blame to them. You will also have a longer recovery time as your leg will not be load bearing for some time, but you will be in possession of the best hip joint there is; your own! What you will likely receive for trauma, even if the fracture is so slightly displaced as to seem much like a 'crack', is the Hemiarthroplasty; the worst of all prostheses, because it's cheap, has a short operating window, and is likely to last five or six years, so they will be beyond the date whereby failure would not be paid for under the tariff.
This has resulted on many occasions in the almost complete lack of hip repairs in trauma patients because of the incidence of failure. This is despite the fact that preservation of the native acetabulum and femoral head is the ideal solution. Failure rates of hip repairs are the subject of much conjecture but they are only about 25% in reasonably healthy people up to 65 or 70 years. They are also quick to do, much less traumatic, and can be undertaken, often without general anaesthetic, and sometimes without incision. Generally this requires nails or screws to fasten the joint together which are then left in place. If this fails, then you can go on to have a full procedure at a more leisurely pace and not as an emergency. But it won't happen, because if it fails, the Hospital involved will not get paid for the subsequent and much more expensive procedure to fix it because the 'system' attributes the blame to them. You will also have a longer recovery time as your leg will not be load bearing for some time, but you will be in possession of the best hip joint there is; your own! What you will likely receive for trauma, even if the fracture is so slightly displaced as to seem much like a 'crack', is the Hemiarthroplasty; the worst of all prostheses, because it's cheap, has a short operating window, and is likely to last five or six years, so they will be beyond the date whereby failure would not be paid for under the tariff.The NHS likes this implant despite it's short life because it also has a lower dislocation rate, can be installed by relatively lowly surgeons and through the side of the hip. This is despite the fact that more damage to the muscles and cartilage ensues in this approach. In addition as this implant simply is a metal ball, sometimes with a plastic floating cup (bipolar version) which is literally 'pushed' into the acetabulum. It also brings in some cash from the Primary Care doctors for monitoring X-rays that have to be taken to check up on wear of the bony cup that is the acetabulum. It's almost beyond belief that anyone would consign a patient to receive a big metal ball 'stuffed' into a bone socket that's absolutely certain to wear away and cause pain in quite short order as it articulates with movement. Metal on bone; it doesn't take a scientist to work out which will wear first, especially in a younger, active patients, now does it? Alright, for the 85 year old with little in the way of exercise and a number of co-morbidity's, it may, just maybe justified after a fall, but as a first line treatment for most it's a cynical manipulation of guidelines and flies in the face of good practise and the welfare of the patient to reap the reward of the tariff.
Hip joints are one of the wonders of nature. They are a 'ball and socket' certainly, but one that has an interference fit that has a regenerative liner of cartilage and a fluid cushion that acts like the hydraulic fluid in a shock absorber, being 'squeezed' out and in as you walk and load the joint. As engineers we haven't even got close to this model nor are we ever likely to. There's no demand, well not from the medic's, the NHS and certainly not Big Pharma's devices wing. The patients, well we're the last people they care about, so long as the 'gravy train' keeps rolling. J and J's rubbish prosthesis is symptomatic of the 'device industry' and the final irony, as I keep hammering on about, is that most of these devices are implanted in women, because the female hip has much more 'articulation' than that of men to enable child birth, rendering their hips more liable to breakage. So women, often elderly women or those viewed as elderly by the NHS are the main recipients especially of 'hemi's', often when they and their peers see them as 'mature'. More misogyny, heavily tinged with ageism. Well there's a surprise!



After reading your comments I wondered if there was a 'gold standard' for hip replacement, since one of the key concerns raised in your analysis was that the NHS was either too stupid, or possibly just plain indifferent to the anticipated benefits of using one device over another - yet it seems, even today, that the jury is still out on a definitive approach, at least to THR?
ReplyDeleteThe study cited below looks at clinical activity beyond the NHS and concludes, "There is limited evidence regarding comparative effectiveness of various hip implant bearings, and the results do not indicate any advantage for metal on metal or ceramic on ceramic implants compared with traditional bearings. A large and high quality randomised controlled trial of bearing surfaces in total hip replacement needs to be conducted before any claims of benefit are made. Until then national registries provide important real world data that are critical for the safety and future comparative safety and effectiveness evaluation".
And, "Disease specific functional outcomes such as Harris hip score and general quality of life measures were no different between patients with metal on metal or ceramic on ceramic hip implants compared with traditional hip implants. There is some evidence of higher rates of revision surgery associated with metal on metal implants compared with metal on polyethylene implants. While an investigational device exemption trial reported fewer revisions associated with ceramic on ceramic implants, the emerging evidence from national registries does not support these results.
http://www.bmj.com/content/343/bmj.d7434
Thanks again for a great blog.
Thanks for a thoughful response.
ReplyDeleteThe essence of my argument is that both the NHS and the myriad of private providers have been captured by the influence of the Medical Device makers in the choice of THR implants, often to the detriment of patient well-being. It is true that many offer little in the way of improvement over any other in terms of Harris Hip Score. But again we are placing huge responsibility upon the patient to factually report their outcomes in a subjective manner from a starting point that is often imbued with pain and suffering. It is unsurprising that in these circumstances their limited expectation of mobility and relief from pain colours their judgement in the rendering of data.
Any 'gold standard'is hard to extract from the study you cite except to say that polyethylene for all it's faults is the least toxic of the materials. But again we face the choice of 'lesser evils' because none are anywhere near an approximation of a standard even approaching 'gold'. Material choice is critical, especially for friction surfaces but the makers goals are centred upon improvements of the implant mechanics instead of questioning the whole concept of THR or indeed whether we should try and emulate natural bone with it's attendant tensile strength with a man made alternative. In other words let's look at the scaffold, before worrying about the boards.
Should we not offer alternatives in the early stages of OA, instead of rushing headlong to the operating theatre for a resolution? In my own case, I have OA in both knees since I was fourty. But by careful physio, Omega 3 supplementation and a life style devoted to dietry interventions I have kept it at bay for twenty years, with little to no pain (now) and no NSAID's except the very occasional use of a topical one if I 'over do' the walking. OA is an increasing risk for all, as is NIDDM and obesity and they are inextricably linked, although in my own case it was the consequence of injury brought about by lifstyle. And on that topic is it not about time that we warned those who undertake marathons, jogging, and high impact sports about the consequences they will face ten or twenty years later instead of hammering on about fat and cholesterol. Sorry, off topic there, but at least smokers just die, joggers get new knees and then start to wear them out all over.
My real gripe is the 'tarrif', the way it works and the fear and consequent lack of skills that is now prevailing in truama as a result. Orthopods will virtually never repair any hip now except a classic undisplaced one in patients below 60 years. And trainees are being brainwashed by their mentors into what they feel is 'best' rather than what is scientific fact. Cement is being used in virtually all all stem fixing with it's attendant cardiac risks because of its expediency in mobilisation, early discharge and lack of need for physio support. The 'longer' view for patient outcomes that are better, is being sacrificed on the altar of surgical intervention. It is sometimes better to take three months to heal rather than six weeks if you retain, at the end native pelvic articulation. And let us not forget, that J and J, Stryker, et al have been charging much more for these 'state of the art' devices that have proven to be so toxic.
Hi
ReplyDeleteThis comment has been removed by the author.
ReplyDeleteThe metal-on-metal hip implants is regarded as a longer lasting hip device but lurking inside its durability is a risk of metallosis. Although DePuy has not issued a warning, nor has it voluntarily initiated recall, controversy has already affected consumer trust in the device. Some recipients have already filed DePuy Pinnacle lawsuit.
ReplyDelete