I left the story last at the juncture where I was trying to fathom what had happened to J' whilst she was in Hospital, and why so many things had gone wrong. I had been trying to convince her, that we needed to both find out exactly what her prosthetic hip, was and to ascertain why she had been so ill postoperatively, at least.
It took some convincing, on my behalf as J' wanted to put it all behind her; to forget all about it completely, whereas I did not. I did quite a lot of soul searching, as I knew that J' continued to display stress when talking about events that had occurred and I did not want to coerce her into anything. It was painful for me too, but I felt it imperative at least to garner some information, so as to guide any action in the future. So the first step was taken; that of requesting all the notes about her Hospital treatment.
What may seem a simple request, turned out to be more difficult than anticipated and I sought the help of the Patient Advocacy Service to assist me in this. I was not confident that they would be of any use but was pleasantly surprised by the case officer appointed, Andrew (not his real name, which I never knew) whose knowledge and understanding was of great help. So we submitted a request for the medical notes and sat back and waited, and waited. Well it took an age, cost some £50 and came in instalments. And of course you have no proof that what you receive is comprehensive, because you do not know what may have been omitted. Some two months later we actually had them all and I commenced the task of review.
Despite my knowledge of Human Biology and Biochemistry, I admit to floundering somewhat; well quite a lot actually. I had not looked into science in this area for more than thirty years (my how time flies) and I found that I not only had to hit the books, but had to buy some more contemporary ones. But of course we now had the Internet, except I had not used it much before, being a bit of a 'luddite' in a way although I had embraced microprocessor logic quite extensively. So now I had to embrace that as well. But after a few hiccups I was soon getting up to speed.
My review of the various tests conducted proved to be the most illuminating element of J' treatment and the memory I had of the Paramedics question, about controlling her Diabetes soon became understood. Her preop' blood glucose was 19.50 mmol/L ! That is severe, uncontrolled hyperglycemia, a situation that could only indicate Type 11 Diabetes. In addition she had been given a 'bolus' of several antibiotics including several penicillin's. She has a well documented adverse reaction to this type of antibiotic, which was advised to the Hospital on admission and it was clearly stated on the notes. There was also strangely, a copy of an ECG trace together with a chest X-ray copy (on disc). These were 'ghosts', because no such procedures were undertaken, and let's face it it would be extremely difficult to 'sneak' an ECG onto a patient, with ten electrodes having to be placed onto various parts of the body and the machine, being wheeled into the cubicle, especially as I was there too. Bizarre is the only word I can use for this.
So the first thing I had to do was to address the distinct possibility of Diabetes. I knew that high blood sugar is symptomatic in trauma patients, it's part of the human stress reaction, but not anything like the levels reported (and ignored!). So I purchased a blood glucose monitor and some test strips and tested J' for both fasting and post prandial (after a meal) levels. I did this on three days to be absolutely certain and the figures were indeed well above normoglycemic levels, in the region of 10mmol/L (fasting). So whilst I was by then sure she was a Type 11 Diabetic, it has to verified by a Doctor for this to be 'official' so we had to make an appointment to see the GP which we did. When we talked to her (the GP) she was also convinced of the same and immediately wrote out a 'scrip' for Metformin. And she gave us a blood test instruction to be fulfilled at either of the two local Hospitals. I viewed this as somewhat premature, but she dismissed totally the concept of diet and exercise as a protocol for containment of the Diabetes. A rush to judgement? Well pretty much I felt, so we did not fill the prescription and never did.
I had already completed some research into Diabetes prior to the GP visit as the only thing that I could recall from College was that the 'Islets of Langerhans' become non-functional and thus produce little to no insulin. J' also had more practical experience than I, as her father had Non Insulin Dependent Diabetes Mellitus (NIDDM) for a large part of his life. But his condition was treated with diet and exercise. That frankly was my take as well because that had been the protocol for most, thirty or more years ago. What had changed it seemed, was the fear of fat and meats, as the diet route dictated that little to no carbohydrate be consumed. As all carbohydrates convert to glucose in the digestive system somewhat rapidly, it also made biological sense to shun them. What had changed then since my studies in the 1960's? Well quite a lot it seemed.
'Big Pharma' in it's ceaseless pursuit of money had become all powerful along with Diabetes UK, an alleged patient advocacy organisation, and their dominance of the treatment paradigm now in place dictated that Diabetics take a cocktail of drugs including it seems Insulin. Insulin Dependent, Non Insulin Dependent Diabetics? Well that seemed somewhat nonsensical. More research was obviously needed and urgently, but we did concentrate our efforts, (for by this time J' was 'onside' about this, if little else), on reducing carbohydrates with a view to elimination.
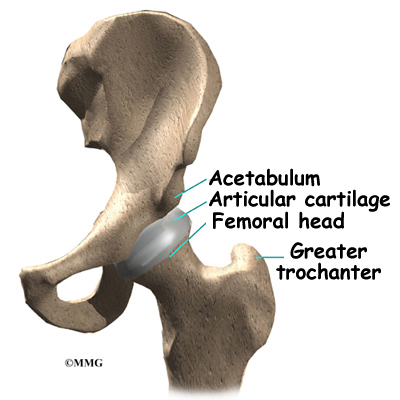
After more heart searching J' finally agreed that we should also register a formal complaint with the Trust about her treatment and now, because of the notes, we also had (at last) found out what 'they' had put inside her (hip). It was a bi-polar hemiarthroplasty, which is a 'hemi' with a plastic cup added to the top of the head (ball), that was 'stuffed' (no other word describes it better) into her acetabulum. Research sadly does not attribute this with any better outcomes than a simple 'hemi' and the recipient also has more plastic debris to cope with together with little in the way of less acetabular erosion or protrusion. So it is little better than a simple 'hemi', just a bit more expensive. It had taken more than four months to determine the presence of this prosthesis, which somewhat flies in the face of so-called 'informed consent' we were alleged to have given.
And so the Complaint System rumbled forward, until we at last had a meeting. I have written about this in detail a while ago and do not propose to go over it again. Suffice to say we were both devastated by the outcome and resolved to pursue things further, but frankly the ground rules kept moving throughout the procedure making it difficult to find our way. The Brown Government, overseen by that most useless of all Health Secretaries, Andy Burnham decided that a change was needed halfway through our complaint, and we were now left with no choice than to complain that we thought we had been dealt with unfairly, and that the 'Local Resolution' system should review the case once more. The response to this was a refusal, leaving the 'last hope', a referral to Parliamentary and Health Service Ombudsman as our final port of call. But at this stage we decided to concentrate on J's various problems and look for as many solutions as we could.
These were; the need to restore her mobility as much as reasonably practicable with the poor prosthesis she had been given.
To control her Diabetes and achieve normoglycemia as much as possible with the minimum of side effects.
And to investigate the pronouncement about her having osteoporosis we found in the notes.
She had a pronounced limp, termed Trendelenburg's Sign, which was placing some strain on her left leg. We needed some physiotherapy intervention for this and, luckily the PCT in the area had a a policy of self-referral, so we did not have to see the GP for this. Using a bit of 'leverage' in my circle of friends, I was able to get her an appointment quickly and we got one of the best in the area. He agreed that J' needed help and devised a work plan that involved resistance exercises that I had to help with, that rebuilt the muscles damaged by the operation. It was hard for her and sometimes painful to see, and often I felt terrible for driving her efforts. But after three long months, it bore fruit and the limp was gone. It also helped with her Diabetes by gist of the exercise needed which reduces insulin resistance in the muscles that helps to lower blood glucose.
Her Diabetes gradually came under control with a low carbohydrate diet, regular exercise with walking and an exercise bicycle, together with a few carefully targeted supplements. Her Hba1c reduced from 8.5 to 6.5 in three months, she lost some weight and the youthfulness she formerly displayed, gradually returned. There was a lot more to achieve as yet, but the walks along the canals helped to keep us both reasonably fit and sane. J' had gone from a vibrant, youthful woman, holding down a well paid job to a partially disabled Diabetic with alleged 'brittle' bones, needing help with at least some aspects of life. She had to have an automatic car, help with getting in and out of bath and could only work part-time.
No one person or organisation was responsible for the accident or the Diabetes, but what the Trust did was to ignore many obvious and relatively simple measures that prejudiced her recovery, her future, her very life even at one point, without any sense of responsibility for their actions and lack of them. No sense of danger in their lax and supine protocols; no remorse, no empathy, but above all no candour and no justice. I had lost my innocence about 'our' NHS, an organisation I had championed in the past, even been grateful to for saving the lives of two of my children. Yet now, after the injection of extra billions in funding, it was actually worse than when it was a service for the poor 'proles' back in 1948. It was devoid of humanity, and the primary tenet governing all that medicine stands for, 'do no harm', because it was doing great harm and 'selling' it as care. It had made an enemy of me and I was to learn in the coming months, many others too. I was no longer 'Winston Smith' and I no longer loved Big Brother.
This saga continues shortly, after I catch my literary breath.
Friday, 23 March 2012
Friday, 16 March 2012
Slicing The Salami (and calling it steak).
 I am taking a brief respite from the 'Loss of Innocence' saga, to excoriate about the publicity for the study about the intake of meats causing Cancer. Much was made of this in the print and broadcast media with precious little criticism or adverse comment from, well anyone. But in truth it was like most of these proselytising studies, that attempt to steer us from the path of our demise by feeding us the results from 'scientific' research that is not really scientific at all.
I am taking a brief respite from the 'Loss of Innocence' saga, to excoriate about the publicity for the study about the intake of meats causing Cancer. Much was made of this in the print and broadcast media with precious little criticism or adverse comment from, well anyone. But in truth it was like most of these proselytising studies, that attempt to steer us from the path of our demise by feeding us the results from 'scientific' research that is not really scientific at all.The study, published in the Archives of Internal Medicine is an observational study, which means it is not presenting any evidence, merely drawing conclusions from data provided by food frequency questionnaire's filled in by the cohort every four years! I can't even remember what I had for dinner last Tuesday, except to know it would have had meat in it; probably lots of it. These epidemiological type studies are really the starting point of a hypothesis to test it's credibility. They are not the end point, merely the beginning of a journey that should encompass all of the checks and balances that science should pursue to ensure that any statement made about anything should at least be founded in proven fact. So, is it likely that the cohort from whom the data was drawn, reported the facts of their diet without telling a few little lies? I really think not, but that's a side issue really.
Let us then look a little deeper. Firstly we see that all meat, processed or otherwise so long as it's red, is alarmingly 'lumped' together, although they do within the study provide some separation of the two and indeed indicate that 'processed' meats are more harmful than other types. But looking further we find that the actual questionnaire lists hamburger meat as 'unprocessed'. You can read about the reliability of Food Frequency Questionnaires here. This highlights the tendency for the cohort to over report socially acceptable foods rather than those they have been 'brainwashed' to reject, but nonetheless still consume. It may also not escaped your attention, that it is the same Institution that also produced this study. Ironic? I could not comment.
So 'hamburger' meat passes for red meat in the US. And to some extent, if you want to give credence to any of this rubbish then remember that the cohort is entirely comprised of US citizens. There is meat, and then there is American meat most of which is 'lot fed' in corrals most of it's life and fed on concentrates of soy protein, cattle corn and antibiotics. It's no longer meat as we know it! Europeans although consuming meat of this type in small amounts, generally eat grass fed beef and lamb, the latter of which is a large part of their 'red meat' diet. So if this study proves anything (and I don't think it does) it proves that eating US meat and all the other elements of the diet, of those who filled in the Questionnaire, could possibly, maybe, cause Cancer. Of course there are numerous confounding factors that go unreported such as, what other elements of the diet examined might be contributory to the conclusions about Cancer? All of the cohort may have also drunk vast amounts of alcohol or worse, coke! They may have all been drug addicts for all we know, because it is unreported.
Looking then at the science, about the higher reported incidence of Cancer in those who ate lots of processed meats. There is a mechanism that could be responsible, and again it's something that predominates more in the US than Europe or the UK, and that's nitrites. They are an additive used in the preservation of hams, sausages, bacon and continental sausage. Sodium Nitrite (E250) is used to add colour but more to prevent the growth of the bacteria Clostridium Botulinum, the cause of botulism.
When man started to preserve meat, natural sea or rock salt and air drying were the main agents, but as we became frightened of salt and to speed up processing we began using chemicals. Preserving salts today have the addition of 0.6% sodium nitrite or the potassium version to guard against botulism because we now turn around the processing of meats so quickly that it is much more probable, well not really (anymore) but it does make the product nice and pink. Many long matured air dried 'artisan' sausages do not need it and it's a good idea to avoid it if possible. It is not much of a poison the Lethal Dose 50% (LD50) is 71mg per kilo for humans but nitrites form nitrosamines, which are carcinogens, if they are heated in cooking at high temperature. The highly acidic environment of the human stomach can also bring about the same condition. So it is usual, and a legal requirement in the US, to add ascorbic acid (Vitamin C) at 550 ppm to preserved meat or any meat treated with nitrites. The acid inhibits the formation of nitrosamines and in fact the incidence of stomach cancer fell significantly in the US after its addition to preservation methods.
It is a good idea not to roast ham or fry bacon so that it is charred or too crisp, or to limit intake. If one does eat bacon crisp, which is the way most like it, then take a Vitamin C supplement, it helps to prevent Cancer anyway and is rarely harmful. Alternatively eat high quality processed meats that do not have nitrites, although you may have to go to some lengths to find them. Nitrites can also be found in many green vegetables and root vegetables especially, so you do not want to overload on these either. Lettuce, Spinach and Radishes contain the most and a significant proportion of this can be attributed to the use of nitrate fertilisers. The more mature the plant the lower the level of nitrite. Organic vegetables are usually lower in nitrites than those grown by the multinational growing cartels.
A rare result of over consumption can bring about methaemoglobinaemia, which robs the haemoglobin of its oxygen absorption capabilities and causes hypoxia (oxygen starvation). But one would have to consume vast amounts of nitrites for this to come about and most cases are due to other causes. Again an intake of Vitamin C is both the treatment for this rare disorder and is protective against nitrosamine being formed from nitrite ingestion. Most animals produce their own Vitamin C to combat this but a few, including man lost this ability at some time in the evolutionary chain. And to get enough of this vitamin, drinking orange juice will not cut it I'm afraid. Orange juice is flavoured with err... orange flavouring, because natural orange flavour only lasts hours. So, the processors have to add it back to the packs and bottles it comes in, otherwise it's orange water. Man cannot get enough from diet of this vitamin in today's nutritional environment unless we supplement or eat targeted foods high in its content with watercress being one of the best. However, most green leafy vegetables including cauliflower provide substantial amounts, but yes are also high in.....nitrites! Oh, just take a pill!
So eating preserved meats does have a mechanism that could be causative of some cancers, because it does actually exist, but frankly you would have to eat really large amounts, on a regular basis. And, the bun surrounding the 'unprocessed' burger meat (sic) is likely to be more harmful. And what country is renowned for it's consumption of burgers and barbecued meats? Might that be the country of origin of the cohort of this study, the USA? Always remember, long suffering reader, that observation (and correlation) does not prove causation.
Loss of innocence (part four) continues shortly.
Wednesday, 14 March 2012
Loss of Innocence (Part 3 -Aftermath)
As I drove away from the Hospital that Friday afternoon I felt euphoric, in that I had repatriated the women I loved from what seemed to me a prison. But I realised almost immediately that some practical and needed changes to our lives would be needed, at least in the short term. What was running through my head, were the words J' had related to me from the physio' she had seen on the third day of her ordeal, that "you know you will have to come back in about five years for a revision, when that wears out". Had she heard right? But surely no-one in her position (the physio) would make such a statement without there being some truth behind it?
The Hospital had provided us with crutches, on loan, but they would be an encumbrance in our small and somewhat over furnished flat. I had then purchased a folding 'zimmer' frame for J' to use in the flat, especially if she was alone. I had also bought a bath seat to enable bathing, which in the short term had not to include much in the way of immersion of the wound. But the first things she yearned for had to addressed. A long awaited visit to the toilet, a decent meal, a good night's sleep and of course, her legs shaved, as she felt like a 'yeti' from the knees down!
Chanting the phrase, 'good to heaven, bad to hell' (which leg, in which order first) she got up the one flight of stairs, with my help. From that day on with me behind going up, in front going down. I do it to this day, although it's importance has waned. Having got her in the flat I padlocked the wheelchair to the banister outside, to ensure it's presence the following day, because there was too little space inside. In fact I removed all extraneous 'trip' spots and paraphernalia from the flat to mitigate the chance of a fall. I then began the process of turning myself into a carer and nurse. In many ways I found it easy; she was so precious to me I did not care about the commitment, or the attention to her intimate needs that were to be thrust upon me. In some ways I welcomed it; she deserved my undivided attention. She had loved and supported me for years and whilst I had always reciprocated, I had without doubt been selfish on many occasions and taken her for granted. I had stood back from myself during those days when I felt such loss and impending doom, and made a pact with her that whatever may become of the future, it would be one where her well being was predominant and not mine, as I felt it had been the opposite for too many years.
And so it began. I bathed her carefully, whilst she sat on the new bath seat. I shaved her legs and she took a mild laxative to reintroduce the process of peristalsis that had been lacking for a week. I got her an extra pillow so as to enable her to be more comfortable and then we had supper; a Chinese meal that she had longed for. Little did I realise, that by pandering to her desire, I was compounding the errors made by the Hospital and pushing her blood glucose through the roof. However that was to be for the future.
It was a blissful weekend in many ways. We went out of town on the Saturday and had a quite lovely meal, with me pushing her into the restaurant in her wheelchair and then helping her into a normal chair, realising as I did it, the problems disabled people had to endure to gain access to so many places. I was to find this irksome after a short while and thus became a harsh critic of establishments that failed to take account of the needs of wheelchair users to enjoy simple pleasures without the need for a small team of weight lifters in accompaniment. How blind we all are to others, when it does not impinge upon our lives. But this bliss was tinged with some sadness. I hoped that J' would be able to walk quite soon, hoped her recovery would be rapid but I also realised that it would be a long hard road and it was likely that she would never be able to ride a horse or a bicycle, partly because the consequence of a fall, with a big metal ball on a stem instead of her greater trochanter, would be too greater risk for me to let her. She had been doing both since she was twelve, and generally viewed horses as superior to humans', most of the time. Then I had to face the problem of my work whilst fulfilling the needs of her carer. It would be a long time in the future when I could leave her alone without a pounding heart.
And so I reached a compromise, at least for the next six weeks before her post-op appraisal. I worked in the mornings and came home in the afternoon to feed her, help with physio exercises and take her out to enjoy what was left of summer. I worked mostly in fear, not really giving it the attention that I should. Ridding myself of the myriad tasks that I had micromanaged before, because my ego would not allow me to delegate to others. I was the only one capable I had always thought, and I lacked the confidence to allow others to fulfil my many roles. But now, I no longer cared about the pursuit of clients or wealth, I just wanted to make her whole again, whatever the cost. It turned out to be high, but I don't think I would have done it differently, even given another chance. Then again all of us often feel that if we needed to start over we wouldn't want to start from here, but we cannot turn back time although on occasions in the next few months, I would often wake up and think it was just a bad dream and I would look to my left and see the J' I used to know, not the one I now had, who always looked as if pain was her only emotion.
We got her stitches removed on the next Monday. late it seems because those damn paper clips that pass for sutures today could hardly be called 'stitches', should have been done at day five apparently as the flesh had started to 'grow' over them. I winced for her as they were dragged from her flesh by the GP Nurse. She re-dressed the wound which was healing well, but still resembled a long, red 'slash' in her thigh. I kept thinking why did it all have to be so disorganised, why was there not some sort of 'plan' for the aftercare of hospital patients? Then I remembered there had been little in the way of plan right at the start. Maybe someone had written it down on the back of a 'fag 'packet somewhere, and then lost it; well that's how it seemed. Everything had the appearance that it was left to 'kismet', rather than any sense of order or commitment to the patients well being.
We took to walking along canal towpaths; they are always flat, except for the locks, and locally there weren't many at all. She would walk with crutches and after some practise, and a little coaching in co-ordination, she became adept. As soon as she tired I would put her in the wheelchair and return from whence we came, back to the little red van. The wheelchair was the 'backstop', the means of letting her learn to walk again, without any risk of not being able to return. Soon she was able to walk with just the one, and one day in late July when I had pushed the chair into the town, as we often did, I purchased for her a 'glamorous' walking cane; all glitter in the handle and a shimmering green on the shaft. After that she cast aside the crutches, and the memory of whence they came; well not quite.
She had been traumatised by what had occurred,to the extent that I could not get her to open up to me about the events to which I was not witness; the pre-op phase, the morning of the operation, the conversations she may (or may not) have had with the Consultant, whom I found out was an expert in, err... hands! It was frustrating, I even got angry a few times, but I realised the depth of harm she had suffered and gave up quite quickly, realising that it was too soon, and that it may never be the right time or perhaps she found it so bad as to have erased it completely.
Eventually the days and hours passed and we came to that moment she hoped for, the day she saw the Consultant. Her main concern being that she could drive once more and return to work. I hoped that he would not allow it, but she put on a 'show'. Still believing, I am sorry to say that this man 'knew what he was doing', and that she wanted to be back where she used to be, and that he would give her license to be so. After ages of waiting we were shown to a cubicle, in the clinic. We sat there for what seemed a long time, me working myself up to a level of stress I had only felt when I was waiting to see if my second child would live, shortly after birth. J' on tenterhooks to see if he would 'sign her off sickness'. Then the great man arrived; all rugby club tie, shiny tan brogues and Oxford striped shirt. What a pr**k he was. Taken aback by my request to see the X-ray, he blustered his way through precisely five minutes, of explanation of what J' should do, which comprised mainly of walking to exercise the leg, but not to bother with any physiotherapy; it wasn't needed. Just "walk up and down for me please, oh that's fine. Any problems go and see the GP". I was still looking at the X-ray and before I could say anything, he was gone!
I had been confused. The image did not compute with that which I expected. Although I had believed J' to have had a hemiarthroplasty, the image showed something that to my untrained eye looked like a total hip arthroplasty. I wanted to quiz the Consultant, but he had already moved on to his next patient; it was the 'little old lady' we had sat next to in the waiting area, and guess what was on the screen at the end of the cubicle? That's right, that same image I had just seen. Even more confusion, or perhaps they just put up the same image for all the screens in the Fracture Clinic, with hip replacements. At that juncture, it would not have surprised me at all.
We left, J' clutching her discharge note, signing her as 'fit to work' together with a letter for the GP (sealed) and me clutching her hand, in a welter of anger, confusion and in need of strong drink. I felt patronised, sidelined and deeply suspicious of the only answer I had gleaned from this Consultant, who seems not to have to consulted in any way with the person(s) with whom he needed, and in answer to the question of "how long will this prosthesis last?", he said, with a straight face, "forever". J' was pleased she had been allowed to drive again and could return to work, which frankly filled me with dread.
She was I realised, simply shutting everything out that she did not wish to face. The events had closed down her usual scepticism and the questioning of matters that she usually displayed, and in it's place was an an almost subservient trusting attitude. It was as if the NHS and Consultants would not undertake any procedure that was likely to provide an outcome that was less than good for a patient. In the coming months that was to change. Change completely, once she found out what they had done, why, and more importantly, what they had forgotten to do. And what they had forgotten was going to impinge upon her life, for all of her life.
Again, dear reader, I crave your indulgence. This story has to be episodic and the 'aftermath' continues again shortly. It is called 'the complaint'.
The Hospital had provided us with crutches, on loan, but they would be an encumbrance in our small and somewhat over furnished flat. I had then purchased a folding 'zimmer' frame for J' to use in the flat, especially if she was alone. I had also bought a bath seat to enable bathing, which in the short term had not to include much in the way of immersion of the wound. But the first things she yearned for had to addressed. A long awaited visit to the toilet, a decent meal, a good night's sleep and of course, her legs shaved, as she felt like a 'yeti' from the knees down!
Chanting the phrase, 'good to heaven, bad to hell' (which leg, in which order first) she got up the one flight of stairs, with my help. From that day on with me behind going up, in front going down. I do it to this day, although it's importance has waned. Having got her in the flat I padlocked the wheelchair to the banister outside, to ensure it's presence the following day, because there was too little space inside. In fact I removed all extraneous 'trip' spots and paraphernalia from the flat to mitigate the chance of a fall. I then began the process of turning myself into a carer and nurse. In many ways I found it easy; she was so precious to me I did not care about the commitment, or the attention to her intimate needs that were to be thrust upon me. In some ways I welcomed it; she deserved my undivided attention. She had loved and supported me for years and whilst I had always reciprocated, I had without doubt been selfish on many occasions and taken her for granted. I had stood back from myself during those days when I felt such loss and impending doom, and made a pact with her that whatever may become of the future, it would be one where her well being was predominant and not mine, as I felt it had been the opposite for too many years.
And so it began. I bathed her carefully, whilst she sat on the new bath seat. I shaved her legs and she took a mild laxative to reintroduce the process of peristalsis that had been lacking for a week. I got her an extra pillow so as to enable her to be more comfortable and then we had supper; a Chinese meal that she had longed for. Little did I realise, that by pandering to her desire, I was compounding the errors made by the Hospital and pushing her blood glucose through the roof. However that was to be for the future.
It was a blissful weekend in many ways. We went out of town on the Saturday and had a quite lovely meal, with me pushing her into the restaurant in her wheelchair and then helping her into a normal chair, realising as I did it, the problems disabled people had to endure to gain access to so many places. I was to find this irksome after a short while and thus became a harsh critic of establishments that failed to take account of the needs of wheelchair users to enjoy simple pleasures without the need for a small team of weight lifters in accompaniment. How blind we all are to others, when it does not impinge upon our lives. But this bliss was tinged with some sadness. I hoped that J' would be able to walk quite soon, hoped her recovery would be rapid but I also realised that it would be a long hard road and it was likely that she would never be able to ride a horse or a bicycle, partly because the consequence of a fall, with a big metal ball on a stem instead of her greater trochanter, would be too greater risk for me to let her. She had been doing both since she was twelve, and generally viewed horses as superior to humans', most of the time. Then I had to face the problem of my work whilst fulfilling the needs of her carer. It would be a long time in the future when I could leave her alone without a pounding heart.
And so I reached a compromise, at least for the next six weeks before her post-op appraisal. I worked in the mornings and came home in the afternoon to feed her, help with physio exercises and take her out to enjoy what was left of summer. I worked mostly in fear, not really giving it the attention that I should. Ridding myself of the myriad tasks that I had micromanaged before, because my ego would not allow me to delegate to others. I was the only one capable I had always thought, and I lacked the confidence to allow others to fulfil my many roles. But now, I no longer cared about the pursuit of clients or wealth, I just wanted to make her whole again, whatever the cost. It turned out to be high, but I don't think I would have done it differently, even given another chance. Then again all of us often feel that if we needed to start over we wouldn't want to start from here, but we cannot turn back time although on occasions in the next few months, I would often wake up and think it was just a bad dream and I would look to my left and see the J' I used to know, not the one I now had, who always looked as if pain was her only emotion.
We got her stitches removed on the next Monday. late it seems because those damn paper clips that pass for sutures today could hardly be called 'stitches', should have been done at day five apparently as the flesh had started to 'grow' over them. I winced for her as they were dragged from her flesh by the GP Nurse. She re-dressed the wound which was healing well, but still resembled a long, red 'slash' in her thigh. I kept thinking why did it all have to be so disorganised, why was there not some sort of 'plan' for the aftercare of hospital patients? Then I remembered there had been little in the way of plan right at the start. Maybe someone had written it down on the back of a 'fag 'packet somewhere, and then lost it; well that's how it seemed. Everything had the appearance that it was left to 'kismet', rather than any sense of order or commitment to the patients well being.
We took to walking along canal towpaths; they are always flat, except for the locks, and locally there weren't many at all. She would walk with crutches and after some practise, and a little coaching in co-ordination, she became adept. As soon as she tired I would put her in the wheelchair and return from whence we came, back to the little red van. The wheelchair was the 'backstop', the means of letting her learn to walk again, without any risk of not being able to return. Soon she was able to walk with just the one, and one day in late July when I had pushed the chair into the town, as we often did, I purchased for her a 'glamorous' walking cane; all glitter in the handle and a shimmering green on the shaft. After that she cast aside the crutches, and the memory of whence they came; well not quite.
She had been traumatised by what had occurred,to the extent that I could not get her to open up to me about the events to which I was not witness; the pre-op phase, the morning of the operation, the conversations she may (or may not) have had with the Consultant, whom I found out was an expert in, err... hands! It was frustrating, I even got angry a few times, but I realised the depth of harm she had suffered and gave up quite quickly, realising that it was too soon, and that it may never be the right time or perhaps she found it so bad as to have erased it completely.
Eventually the days and hours passed and we came to that moment she hoped for, the day she saw the Consultant. Her main concern being that she could drive once more and return to work. I hoped that he would not allow it, but she put on a 'show'. Still believing, I am sorry to say that this man 'knew what he was doing', and that she wanted to be back where she used to be, and that he would give her license to be so. After ages of waiting we were shown to a cubicle, in the clinic. We sat there for what seemed a long time, me working myself up to a level of stress I had only felt when I was waiting to see if my second child would live, shortly after birth. J' on tenterhooks to see if he would 'sign her off sickness'. Then the great man arrived; all rugby club tie, shiny tan brogues and Oxford striped shirt. What a pr**k he was. Taken aback by my request to see the X-ray, he blustered his way through precisely five minutes, of explanation of what J' should do, which comprised mainly of walking to exercise the leg, but not to bother with any physiotherapy; it wasn't needed. Just "walk up and down for me please, oh that's fine. Any problems go and see the GP". I was still looking at the X-ray and before I could say anything, he was gone!
I had been confused. The image did not compute with that which I expected. Although I had believed J' to have had a hemiarthroplasty, the image showed something that to my untrained eye looked like a total hip arthroplasty. I wanted to quiz the Consultant, but he had already moved on to his next patient; it was the 'little old lady' we had sat next to in the waiting area, and guess what was on the screen at the end of the cubicle? That's right, that same image I had just seen. Even more confusion, or perhaps they just put up the same image for all the screens in the Fracture Clinic, with hip replacements. At that juncture, it would not have surprised me at all.
We left, J' clutching her discharge note, signing her as 'fit to work' together with a letter for the GP (sealed) and me clutching her hand, in a welter of anger, confusion and in need of strong drink. I felt patronised, sidelined and deeply suspicious of the only answer I had gleaned from this Consultant, who seems not to have to consulted in any way with the person(s) with whom he needed, and in answer to the question of "how long will this prosthesis last?", he said, with a straight face, "forever". J' was pleased she had been allowed to drive again and could return to work, which frankly filled me with dread.
She was I realised, simply shutting everything out that she did not wish to face. The events had closed down her usual scepticism and the questioning of matters that she usually displayed, and in it's place was an an almost subservient trusting attitude. It was as if the NHS and Consultants would not undertake any procedure that was likely to provide an outcome that was less than good for a patient. In the coming months that was to change. Change completely, once she found out what they had done, why, and more importantly, what they had forgotten to do. And what they had forgotten was going to impinge upon her life, for all of her life.
Again, dear reader, I crave your indulgence. This story has to be episodic and the 'aftermath' continues again shortly. It is called 'the complaint'.
Friday, 9 March 2012
Loss of Innocence (On the Ward)
That night felt as if it would last forever, despite it being the longest day. Like all things in life, however it did, and dawn crept over the trees in J's garden. I must have dozed for a couple of hours, at some time but my mind kept taking me through events, past and present, in some sort of search to find reasons, solutions, maybe even absolution for my perceived guilt. It had been my idea to take up cycling; I had bought her the bloody bike!
As soon as I thought it late enough for the ward to awake I rang, and rang, but no-one answered. Then after many attempts it was finally answered and I was told J' was already on her way to theatre, and I should have rung earlier! Stifling the expletives, I asked when they would know if she was OK and was told to ring back at midday. I tried to calm my stress and rationalise the risks as I always told others to do, but it didn't work, so I busied myself sorting out her glasses, her 'phone and fresh underwear. I wanted to be the first face she would see on awakening, but I was beset with a dread that that would not even happen.
The walls were closing in and after calling in to be taken off standby I drove down the hill once more to get as close to her as I could. I had 'phoned an old surgeon friend earlier to get advice and he had helped a bit but I sensed some tension in his voice, and was to learn later that he had become an arch enemy of the Trust after his wife had died there due to misdiagnosis some months before. He had given me some sage advice and I guessed he didn't want to depress me too much by relating his woe's, at the time. I rang at midday and surprisingly the 'phone was answered quickly and I was told J' was out of theatre and would be on the ward by visiting at 2pm. Emotion washed over me like a tide; she was alive! I used my 'borrowed' staff pass and parked in the empty car park at geriatrics. I walked then to the entrance and sat down to wait out the time, clutching my plastic carrier of donations to her future comfort. She was alive at least; I had that to be grateful for and surely nothing else could go wrong, could it?
I entered the ward just as they unlocked the doors; her bed was curtained off. I entered and there propped up on pillows was my love. She looked terrible, so small, oxygen mask on, IV drip, four other lines and oximeter and BP monitor permanently connected. I kissed her and she opened her eyes and smiled wanly at me.She was very dopey and kept drifting off as I talked to her. I was quite concerned about her health; something was not quite right. I checked the BP monitor and pulse and pressure were very low (hypo tension). Oxygen saturation was also pretty poor, hence the oxygen mask. She seemed somewhat more ill than I had anticipated or that my friend had suggested to be likely. I put it down to an adverse reaction to anaesthesia but I was later (much later) to find it was due to inadequate preoperative assessment and lack of care.
About two hours after my arrival a nursing assistant entered the curtains and ran a check on the machinery and entered it on a chart I realised was at the bottom of the bed. As soon as she was gone I looked at it. Fifteen minute 'obs' (observations) was listed; that obviously wasn't happening! J' was violently sick shortly after and she told me that had been happening since she arrived back on the ward. I told her it was quite normal especially after morphine administration. As she became less sleepy I tried to find out what had transpired prior to the operation and after. She knew very little except she had seen a Consultant for a few minutes and an Anaesthetists very early that morning, but was unaware of what had been done, or the type of implant. She was somewhat tearful and I realised that it had been very traumatic for her, unsurprisingly and I pressed her no more. All too soon the bell rang for the end of visiting and I had to leave her again, in that awful place.
It was a dump. Hot, humid with no cold drinking water. Down at heel, with floor tiles missing, curtains hanging off rails, immensely noisy and food that had a remarkable similarity to, well,' pig swill'. I began to wonder what all that extra money we had given the NHS had been spent on. It certainly wasn't the infrastructure or patient comfort, and staffing levels were appallingly low. I spoke with the 'ward manager' on my way out but pretty much got 'brushed off' with platitudes and little else; she had no knowledge of what J's prosthesis was and suggested I speak with a Doctor, but one wasn't available. This pretty much remained the theme of most of J's stay.
I emerged into the late evening sunshine and drove back up the hill. Not wanting to go back to the empty flat I went to see Rob and Sandra, my friends who ran a local pub. Sandra insisted on feeding me and as I sat with them I related my tale of woe. They were kind and sympathetic, expressing genuine concern for J' and slightly heartened I decided to go home and do something. I 'phoned the Hospital communications provider (which went bust a few weeks later) and set up an account so that J' had television and a 'phone. I couldn't believe the expense; there was a daily charge of £5 plus call charges of 50p a minute, even then incoming calls were also charged, so you paid twice! I was past caring then so I put a £100 credit on my card and tried to rest.
I wasn't very successful and kept waking up in a cold sweat, fearing for both our futures, especially what outcome J' would have and when I could retrieve her from that awful place. I got up at dawn and tried to fill my day until visiting. I got her a newspaper and some cold bottled water and put it into a 'cool bag'. I bought some snack foods to pad out her diet little realising that that which I chose was likely to add to her illness, but that was something for the future. I made my way back to the ward and there she was still on the oxygen! The drip had gone but all the IVs were still in place, all five; two in the anticubital fossa, which is uncomfortable, even painful. She was at least brighter and more animated, but I was still concerned that pulse-ox was permanently in place and the BP cuff. She said no-one had been near her all day to talk to her or get her out of bed and the wound had bled profusely in the night, needing her to be changed twice. Her old knee injury was hurting a lot due to the leg being flat and I showed her how to adjust the contour of the mattress to impart a little bending of the knee and it eased her pain. I set up the television and 'phone and made a note of the number so I could call her before 'lights out' that night. At least now we could keep in touch. At 8pm I again had to leave. Sunday was drawing to close and I had to cope with work tomorrow and I didn't know if I could.
Once home I tried to watch TV without success. I talked on the phone to Doris, her friend from the office and gave her a progress report. She said she would try to get in to see J' on Monday. I tried to read a book, something I have done daily for most of my life, to ease stress but I couldn't. At last the time to 'phone J' arrived and I did. It took forever because the system takes you through an interminable menu and sales nonsense all at some ludicrous cost (to you) despite the fact that you have paid already! She answered me, and I talked with her for a few minutes mindful that the credit was reducing at alarming speed. She said she did feel a bit better but she still had the oxygen. I told her I loved her and wished her goodnight and signed off. I tried sleep again and went off quickly only to awake shortly after with the 'terrors' again.
Monday dawned and I got into the office early. I asked my daughter to take on some of my workload and sensed a lot of resentment, but she reluctantly agreed although I still had to keep my 'phone on in case of emergencies. She was going to like it even less when I took to leaving at 2pm every day but that was for the future. I was off like a greyhound out of the trap at two, and raced to the hospital. Parking was a nightmare as it a weekday and everywhere was full. So I found a spot half a mile away, and now late, I hurried to the ward.
She was still in bed, she still had oxygen! I was getting really worried now, but saw that at least the flow rate had been lowered. J' said she had been up and was allowed to use a 'zimmer' to get to the toilet, which made her feel better. She was concerned about her hygiene as she'd had no real wash beyond a wipe with a flannel since arriving and her legs needed shaving! Doris arrived and brought her some biscuits and we whiled away the time until the end of visiting; me not wanting to press J' about her treatment anymore. She kept telling me that they know what they are doing and I shouldn't be so critical. Doris let me have a few moments alone with J' before I had to leave, so kissed her goodbye and went out the door. Doris was waiting for me, so we could exit together. As I related what had happened in more detail, I started to cry. I couldn't stop myself and I was sobbing by the time we reached the outside air. That big, lovely woman encircled me in her arms and we both stood there weeping, for what seemed an age. Although we had never met before (although we had talked on the 'phone) she had driven miles to get here, after work, when she hates driving, can't park for toffee and can't afford the fuel. The kindness of strangers, it floors me sometimes.
The days and hours crawled by, with me spending six hours a day with J'. What I saw on that ward was appalling. Many 'inmates', as we started to label them, had been there months. Most were quite elderly, some very astute but a lot in early and late stage dementia with broken bones and many comorbidities. Some had been there for months and the lack of sympathetic care, even any care astounded me. Many were left sobbing, even screaming for hours. Some of the relations were plugging the deficit of care by providing it themselves, including feeding, washing, and quite high levels of nursing that the NHS at this trust seemed unwilling or unable to provide. An old friend of J's who actually worked, there castigated me for mounting a 'vigil' at J's bedside and I'm afraid I took that badly, and avoided her for the next year as a result. And yet I had saved that woman's leg a year before, when she broke it in a home fall, lay groaning on the floor for twelve hours until I heard her calls for help and then told her it was broken, when she thought it was just sprained (it's not rocket science). It took a lot of persuading to get her to go to hospital where she found it was almost beyond saving. She had DVT and spent the next three weeks there and has been on Warfarin ever since.
After that Monday J' progressed rapidly, soon learning to walk with crutches. They didn't want to let her go and I had many arguments with the physio's about that as I knew she had to get out of there before she succumbed to some infection, or actually starved. She also hadn't defecated for six days, due to the opiate's. Her BP was still low and I at last realised why; they were pumping ultra low molecular weight heparin into her stomach wall every day, despite her moving about most of the day. And, she still had all the IV's in place at day six! On that day a male nurse, an actual 'real nurse' was on the ward, and I drew his attention to this. He went ballistic! Those lines were out straightaway together with his apology for the tardiness of his colleagues. I went to see the phsio' then and told them I was collecting J' the following day, whatever they said. I don't think they took me seriously but I told the 'ward manager' as well and told them to get the discharge documents sorted otherwise we would go without them. The physio's all seemed to be frankly bloody useless. Beyond teaching J' to walk with crutches and how to cope with stairs, they did stuff all. They didn't even give her any warnings about dislocation avoidance protocols or any after care routines, but I had that in hand. The ward didn't even have a wheelchair available so she was expected to walk half a mile to the entrance, on crutches!
On the discharge day, the Friday, a week after the accident, armed with a wheelchair from the Red Cross, bless 'em, I arrived at the main entrance and parked in a visitor bay with my little red van with the Red Cross sticker displayed. The security guard soon shut up when I told him a I was collecting a disabled patient in a wheelchair, so trundling the chair before me I set off to free my love from the tyranny of the Trust. What a palaver it was as well. Nothing was completed, papers had to be signed, drugs provided for analgesia, a litany of checklists and forms that do nothing to advance the patients care but fulfil the 'tick box' mentality of the empire building management, that was now in charge of this huge teaching hospital. After more than an an hour we set off with me remarking to the cleaner, on our way out that we were making a 'break for the wire', I pushed J' through the corridors to the real world and out into into the sunshine; escape! I got her carefully into the passenger seat of the van, stowed and folded the chair, we were to need for the next three months and drove off. At that moment I was happier than I had been for years. We had escaped the clutches of the NHS, at least for the moment. The aftermath was yet to come and it would be a long time before my love would even approach her previous mobility, but a first step had been taken on a long road that was to test our courage, our relationship, even our sanity.
This is the second instalment of the saga (sorry about the length), that was to unfold over the next months even years. I will post the next instalment shortly, I've called it Aftermath.
As soon as I thought it late enough for the ward to awake I rang, and rang, but no-one answered. Then after many attempts it was finally answered and I was told J' was already on her way to theatre, and I should have rung earlier! Stifling the expletives, I asked when they would know if she was OK and was told to ring back at midday. I tried to calm my stress and rationalise the risks as I always told others to do, but it didn't work, so I busied myself sorting out her glasses, her 'phone and fresh underwear. I wanted to be the first face she would see on awakening, but I was beset with a dread that that would not even happen.
The walls were closing in and after calling in to be taken off standby I drove down the hill once more to get as close to her as I could. I had 'phoned an old surgeon friend earlier to get advice and he had helped a bit but I sensed some tension in his voice, and was to learn later that he had become an arch enemy of the Trust after his wife had died there due to misdiagnosis some months before. He had given me some sage advice and I guessed he didn't want to depress me too much by relating his woe's, at the time. I rang at midday and surprisingly the 'phone was answered quickly and I was told J' was out of theatre and would be on the ward by visiting at 2pm. Emotion washed over me like a tide; she was alive! I used my 'borrowed' staff pass and parked in the empty car park at geriatrics. I walked then to the entrance and sat down to wait out the time, clutching my plastic carrier of donations to her future comfort. She was alive at least; I had that to be grateful for and surely nothing else could go wrong, could it?
I entered the ward just as they unlocked the doors; her bed was curtained off. I entered and there propped up on pillows was my love. She looked terrible, so small, oxygen mask on, IV drip, four other lines and oximeter and BP monitor permanently connected. I kissed her and she opened her eyes and smiled wanly at me.She was very dopey and kept drifting off as I talked to her. I was quite concerned about her health; something was not quite right. I checked the BP monitor and pulse and pressure were very low (hypo tension). Oxygen saturation was also pretty poor, hence the oxygen mask. She seemed somewhat more ill than I had anticipated or that my friend had suggested to be likely. I put it down to an adverse reaction to anaesthesia but I was later (much later) to find it was due to inadequate preoperative assessment and lack of care.
About two hours after my arrival a nursing assistant entered the curtains and ran a check on the machinery and entered it on a chart I realised was at the bottom of the bed. As soon as she was gone I looked at it. Fifteen minute 'obs' (observations) was listed; that obviously wasn't happening! J' was violently sick shortly after and she told me that had been happening since she arrived back on the ward. I told her it was quite normal especially after morphine administration. As she became less sleepy I tried to find out what had transpired prior to the operation and after. She knew very little except she had seen a Consultant for a few minutes and an Anaesthetists very early that morning, but was unaware of what had been done, or the type of implant. She was somewhat tearful and I realised that it had been very traumatic for her, unsurprisingly and I pressed her no more. All too soon the bell rang for the end of visiting and I had to leave her again, in that awful place.
It was a dump. Hot, humid with no cold drinking water. Down at heel, with floor tiles missing, curtains hanging off rails, immensely noisy and food that had a remarkable similarity to, well,' pig swill'. I began to wonder what all that extra money we had given the NHS had been spent on. It certainly wasn't the infrastructure or patient comfort, and staffing levels were appallingly low. I spoke with the 'ward manager' on my way out but pretty much got 'brushed off' with platitudes and little else; she had no knowledge of what J's prosthesis was and suggested I speak with a Doctor, but one wasn't available. This pretty much remained the theme of most of J's stay.
I emerged into the late evening sunshine and drove back up the hill. Not wanting to go back to the empty flat I went to see Rob and Sandra, my friends who ran a local pub. Sandra insisted on feeding me and as I sat with them I related my tale of woe. They were kind and sympathetic, expressing genuine concern for J' and slightly heartened I decided to go home and do something. I 'phoned the Hospital communications provider (which went bust a few weeks later) and set up an account so that J' had television and a 'phone. I couldn't believe the expense; there was a daily charge of £5 plus call charges of 50p a minute, even then incoming calls were also charged, so you paid twice! I was past caring then so I put a £100 credit on my card and tried to rest.
I wasn't very successful and kept waking up in a cold sweat, fearing for both our futures, especially what outcome J' would have and when I could retrieve her from that awful place. I got up at dawn and tried to fill my day until visiting. I got her a newspaper and some cold bottled water and put it into a 'cool bag'. I bought some snack foods to pad out her diet little realising that that which I chose was likely to add to her illness, but that was something for the future. I made my way back to the ward and there she was still on the oxygen! The drip had gone but all the IVs were still in place, all five; two in the anticubital fossa, which is uncomfortable, even painful. She was at least brighter and more animated, but I was still concerned that pulse-ox was permanently in place and the BP cuff. She said no-one had been near her all day to talk to her or get her out of bed and the wound had bled profusely in the night, needing her to be changed twice. Her old knee injury was hurting a lot due to the leg being flat and I showed her how to adjust the contour of the mattress to impart a little bending of the knee and it eased her pain. I set up the television and 'phone and made a note of the number so I could call her before 'lights out' that night. At least now we could keep in touch. At 8pm I again had to leave. Sunday was drawing to close and I had to cope with work tomorrow and I didn't know if I could.
Once home I tried to watch TV without success. I talked on the phone to Doris, her friend from the office and gave her a progress report. She said she would try to get in to see J' on Monday. I tried to read a book, something I have done daily for most of my life, to ease stress but I couldn't. At last the time to 'phone J' arrived and I did. It took forever because the system takes you through an interminable menu and sales nonsense all at some ludicrous cost (to you) despite the fact that you have paid already! She answered me, and I talked with her for a few minutes mindful that the credit was reducing at alarming speed. She said she did feel a bit better but she still had the oxygen. I told her I loved her and wished her goodnight and signed off. I tried sleep again and went off quickly only to awake shortly after with the 'terrors' again.
Monday dawned and I got into the office early. I asked my daughter to take on some of my workload and sensed a lot of resentment, but she reluctantly agreed although I still had to keep my 'phone on in case of emergencies. She was going to like it even less when I took to leaving at 2pm every day but that was for the future. I was off like a greyhound out of the trap at two, and raced to the hospital. Parking was a nightmare as it a weekday and everywhere was full. So I found a spot half a mile away, and now late, I hurried to the ward.
She was still in bed, she still had oxygen! I was getting really worried now, but saw that at least the flow rate had been lowered. J' said she had been up and was allowed to use a 'zimmer' to get to the toilet, which made her feel better. She was concerned about her hygiene as she'd had no real wash beyond a wipe with a flannel since arriving and her legs needed shaving! Doris arrived and brought her some biscuits and we whiled away the time until the end of visiting; me not wanting to press J' about her treatment anymore. She kept telling me that they know what they are doing and I shouldn't be so critical. Doris let me have a few moments alone with J' before I had to leave, so kissed her goodbye and went out the door. Doris was waiting for me, so we could exit together. As I related what had happened in more detail, I started to cry. I couldn't stop myself and I was sobbing by the time we reached the outside air. That big, lovely woman encircled me in her arms and we both stood there weeping, for what seemed an age. Although we had never met before (although we had talked on the 'phone) she had driven miles to get here, after work, when she hates driving, can't park for toffee and can't afford the fuel. The kindness of strangers, it floors me sometimes.
The days and hours crawled by, with me spending six hours a day with J'. What I saw on that ward was appalling. Many 'inmates', as we started to label them, had been there months. Most were quite elderly, some very astute but a lot in early and late stage dementia with broken bones and many comorbidities. Some had been there for months and the lack of sympathetic care, even any care astounded me. Many were left sobbing, even screaming for hours. Some of the relations were plugging the deficit of care by providing it themselves, including feeding, washing, and quite high levels of nursing that the NHS at this trust seemed unwilling or unable to provide. An old friend of J's who actually worked, there castigated me for mounting a 'vigil' at J's bedside and I'm afraid I took that badly, and avoided her for the next year as a result. And yet I had saved that woman's leg a year before, when she broke it in a home fall, lay groaning on the floor for twelve hours until I heard her calls for help and then told her it was broken, when she thought it was just sprained (it's not rocket science). It took a lot of persuading to get her to go to hospital where she found it was almost beyond saving. She had DVT and spent the next three weeks there and has been on Warfarin ever since.
After that Monday J' progressed rapidly, soon learning to walk with crutches. They didn't want to let her go and I had many arguments with the physio's about that as I knew she had to get out of there before she succumbed to some infection, or actually starved. She also hadn't defecated for six days, due to the opiate's. Her BP was still low and I at last realised why; they were pumping ultra low molecular weight heparin into her stomach wall every day, despite her moving about most of the day. And, she still had all the IV's in place at day six! On that day a male nurse, an actual 'real nurse' was on the ward, and I drew his attention to this. He went ballistic! Those lines were out straightaway together with his apology for the tardiness of his colleagues. I went to see the phsio' then and told them I was collecting J' the following day, whatever they said. I don't think they took me seriously but I told the 'ward manager' as well and told them to get the discharge documents sorted otherwise we would go without them. The physio's all seemed to be frankly bloody useless. Beyond teaching J' to walk with crutches and how to cope with stairs, they did stuff all. They didn't even give her any warnings about dislocation avoidance protocols or any after care routines, but I had that in hand. The ward didn't even have a wheelchair available so she was expected to walk half a mile to the entrance, on crutches!
On the discharge day, the Friday, a week after the accident, armed with a wheelchair from the Red Cross, bless 'em, I arrived at the main entrance and parked in a visitor bay with my little red van with the Red Cross sticker displayed. The security guard soon shut up when I told him a I was collecting a disabled patient in a wheelchair, so trundling the chair before me I set off to free my love from the tyranny of the Trust. What a palaver it was as well. Nothing was completed, papers had to be signed, drugs provided for analgesia, a litany of checklists and forms that do nothing to advance the patients care but fulfil the 'tick box' mentality of the empire building management, that was now in charge of this huge teaching hospital. After more than an an hour we set off with me remarking to the cleaner, on our way out that we were making a 'break for the wire', I pushed J' through the corridors to the real world and out into into the sunshine; escape! I got her carefully into the passenger seat of the van, stowed and folded the chair, we were to need for the next three months and drove off. At that moment I was happier than I had been for years. We had escaped the clutches of the NHS, at least for the moment. The aftermath was yet to come and it would be a long time before my love would even approach her previous mobility, but a first step had been taken on a long road that was to test our courage, our relationship, even our sanity.
This is the second instalment of the saga (sorry about the length), that was to unfold over the next months even years. I will post the next instalment shortly, I've called it Aftermath.
Labels:
Crutches,
Dementia,
Fossa,
IV's,
Physiotherapy,
Wheelchair
Thursday, 1 March 2012
Loss of Innocence (Part One- Addendum)
It was my intention to move straight to my second instalment of the saga of J's treatment at the hands of the NHS and in particular the part played by the 'Orthopod's'. However, the intervention of the furore relating to prosthetic hips has given me the opportunity to vent my spleen about the ridiculous situation that exists in the treatment of those unfortunate enough to need any form of hip surgery.
You would think that in view of the large number of procedures undertaken in the NHS that the science would be driving the procedure, when in fact it is more custom and practise tinged heavily with vested interests and hubris. Orthopods (Orthopaedic Surgeon's) are generally viewed by Medicine, even other Surgeons as lacking in subtlety and intelligence. My view is somewhat more colourful and I view them as 'butchers' more than surgeons. Sure, it's a hard job, requiring physical strength and endurance, almost as much as skill because of the need to saw, hammer, drill and slice, with instruments more akin to a construction site and a butchers shop than an operating theatre. And the repair (or often not) of damaged hips epitomises this more than any other procedure. Dealing with hip trauma is probably the most difficult and dangerous procedure any surgeon undertakes. It is important then that the patient is paramount in the evaluation of which path to pursue as regards the protocol that is most efficacious.
It is not beyond my purview that many 'orthopods' are failed Rugby players, not that I attach any significance to that, except to say that their adherence to scientific evidence as a tenet of their professional conduct is perhaps somewhat lacking. It may sometimes be evident that their judgement of certain medical devices might be coloured by the presentation they last 'endured' in Barbados about the latest implantable device from one of the many makers of such engineering masterpieces (sic). One of these, of course is Depuy, a subsidiary of Johnson and Johnson (a family company). They make the 'Pinnacle' implant, which is a MOM (metal on metal) device using cobalt chrome, and this has been indicted as being subject to early failure. And more importantly, (I feel) of causing the migration into the bloodstream, bone and other tissues, of wear particles that are potentially life threatening in a number of ways.
The BMJ in conjunction with Newsnight undertook a study recently that highlighted this problem that is faced by a number of 'younger' patients who have been ill served by the installation of this design of prosthesis into their acetabulum. In truth the BMJ article is somewhat more comprehensive in it's condemnation of the device than was Paxman in the interview with the head 'honcho' of the MHRA who, it would seem had full knowledge of the 2010 recall by Depuy of it's ASR implant (Pinnacle) but seems to have done little about it. Nonetheless I did enjoy Paxman's taking Kent Wood's to task about the fundamentally supine attitude of his organisation when it comes to 'approving' medical devices, which essentially amounts to a review of the specification provided by the makers, because there are few if any clinical trials undertaken, except using the patient cohort as 'guinea pigs'.
As an engineer first and biologist second (but linking the two), I cannot understand how anyone would recommend the installation of any ball and socket device, in the human made from cobalt chrome that will be subject to metal on metal wear or indeed any frictional wear. The cobalt element of the material does have high strength, coupled with excellent corrosion resistance, but whilst it's salts are used by most animals especially ruminants, at high levels it can be toxic and it's compounds have been responsible for cardiomyopathy (heart muscle disease) in humans. Chromium is also quite toxic in its (VI) form except at very low levels and is a known carcinogen as well as being responsible for damage to the kidneys, liver and blood cells. Having said that, if this material had only been utilised for non-frictional component parts it is unlikely that there would have been a problem, but friction in metal to metal bearings throws off metal ions, eroding interfaces which increases gaps in mating surfaces thus introducing 'free play'. This is of course exponential, so the more wear the more the acceleration of that wear. The consequent contamination of the tissue surrounding the acetabulum and femoral stem and migration of these metal ions into the bloodstream promotes high levels of bone loss, cement collar erosion, cartilage damage, and many other toxic side effects that have yet to be fully evaluated.
When you introduce any 'foreign' body or substance into any living organism you have to be very sure that by so doing you are not making matters worse, but obviously this did not seem to impinge upon the corporate 'psyche' of J and J. Greed seems to have been the driving force and don't forget this company had last quarter earnings of $16.3 billion despite having to pay out $3 billion for the Pinnacle debacle in the US.
 This design of implant was targeted at the younger audience and was sold as a 'low wear' prosthetic so as to avoid the need for revision surgery because this cohort tends to be physically very active. Activity promotes wear in any joint be it in humans' or in machinery, unless you can regularly lubricate that joint. There is some value in the concept of synovial fluid performing this function (the hip joints natural lubricant and hydraulic 'cushion'), but as this 'capsule' has effectively to be 'burst' during surgery for access, it is unlikely to function as it was designed by nature thereafter. The simple truth is that in our haste to address the increasing needs of an ageing and increasingly joint challenged society we have lost sight of many of the needs attendant upon the production of manufactured joints for implanting. And sadly it is not just in the metal to metal prosthetics that we have a problem.Many different materials have been tried over the years, especially plastics, sintered metals and ceramics. If one views success as being a bearing surface that does not wear out at all, and what wear does take place as being entirely benign, manufacturers have failed. Failed miserably in this context because all arthroplasty components have a finite life, so except in elderly patients, they are unlikely not to need revision at least once and in young patients possibly more.
This design of implant was targeted at the younger audience and was sold as a 'low wear' prosthetic so as to avoid the need for revision surgery because this cohort tends to be physically very active. Activity promotes wear in any joint be it in humans' or in machinery, unless you can regularly lubricate that joint. There is some value in the concept of synovial fluid performing this function (the hip joints natural lubricant and hydraulic 'cushion'), but as this 'capsule' has effectively to be 'burst' during surgery for access, it is unlikely to function as it was designed by nature thereafter. The simple truth is that in our haste to address the increasing needs of an ageing and increasingly joint challenged society we have lost sight of many of the needs attendant upon the production of manufactured joints for implanting. And sadly it is not just in the metal to metal prosthetics that we have a problem.Many different materials have been tried over the years, especially plastics, sintered metals and ceramics. If one views success as being a bearing surface that does not wear out at all, and what wear does take place as being entirely benign, manufacturers have failed. Failed miserably in this context because all arthroplasty components have a finite life, so except in elderly patients, they are unlikely not to need revision at least once and in young patients possibly more.
UHMWPE has been the material of choice especially the newer 'crosslinked' varieties, for the manufacture of joint surfaces for some years now. Ultra high molecular weight polyethylene displays admirable self lubricating properties together little moisture absorption and considerable strength. But combinations of both this, ceramics and other metals have been tried, to come up with this goal of the perfect implant. None, including UHMWPE is devoid of particulate contamination of the tissue and blood of the recipient, although this last one is probably more benign than others. None are entirely so, and all wear is at a rate in proportion to the amount of use. So active people wear their implants out quicker.
As regards the NHS; well they invariably go for the cheapest they can get away with, THA (total hip arthroplasty) using cemented stems and UHMWPE bearing surfaces is usually the type most will get for either trauma repair or elective surgery, generally for osteoarthritis of the hip. Except for non-displaced or slightly displaced fractures, when the waters become extremely muddied. This is because of the payment system that prevails in trauma care which is based on a tariff for the most expensive treatment involved in a hospital 'stay', and the desire to keep the costs low, avoid re-admission and get rid of you as soon as possible. Trauma patients 'bugger up' the system, take up unplanned beds and play havoc with operating lists and theatre time allocations. If you aren't fixed quickly it costs more than the tariff. If they do something that's possibly short term, even if it's in your best interest as a patient, it's likely not to happen. If you are re-admitted for something that's a result of your initial admission, they won't get paid for it, so you are a burden.
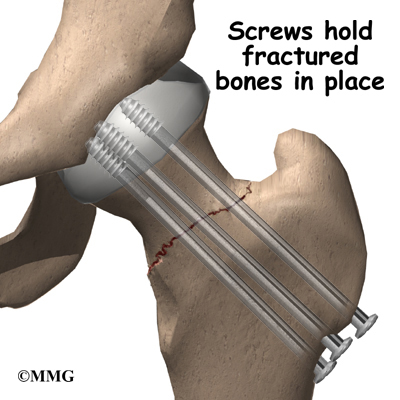 This has resulted on many occasions in the almost complete lack of hip repairs in trauma patients because of the incidence of failure. This is despite the fact that preservation of the native acetabulum and femoral head is the ideal solution. Failure rates of hip repairs are the subject of much conjecture but they are only about 25% in reasonably healthy people up to 65 or 70 years. They are also quick to do, much less traumatic, and can be undertaken, often without general anaesthetic, and sometimes without incision. Generally this requires nails or screws to fasten the joint together which are then left in place. If this fails, then you can go on to have a full procedure at a more leisurely pace and not as an emergency. But it won't happen, because if it fails, the Hospital involved will not get paid for the subsequent and much more expensive procedure to fix it because the 'system' attributes the blame to them. You will also have a longer recovery time as your leg will not be load bearing for some time, but you will be in possession of the best hip joint there is; your own! What you will likely receive for trauma, even if the fracture is so slightly displaced as to seem much like a 'crack', is the Hemiarthroplasty; the worst of all prostheses, because it's cheap, has a short operating window, and is likely to last five or six years, so they will be beyond the date whereby failure would not be paid for under the tariff.
This has resulted on many occasions in the almost complete lack of hip repairs in trauma patients because of the incidence of failure. This is despite the fact that preservation of the native acetabulum and femoral head is the ideal solution. Failure rates of hip repairs are the subject of much conjecture but they are only about 25% in reasonably healthy people up to 65 or 70 years. They are also quick to do, much less traumatic, and can be undertaken, often without general anaesthetic, and sometimes without incision. Generally this requires nails or screws to fasten the joint together which are then left in place. If this fails, then you can go on to have a full procedure at a more leisurely pace and not as an emergency. But it won't happen, because if it fails, the Hospital involved will not get paid for the subsequent and much more expensive procedure to fix it because the 'system' attributes the blame to them. You will also have a longer recovery time as your leg will not be load bearing for some time, but you will be in possession of the best hip joint there is; your own! What you will likely receive for trauma, even if the fracture is so slightly displaced as to seem much like a 'crack', is the Hemiarthroplasty; the worst of all prostheses, because it's cheap, has a short operating window, and is likely to last five or six years, so they will be beyond the date whereby failure would not be paid for under the tariff.
The NHS likes this implant despite it's short life because it also has a lower dislocation rate, can be installed by relatively lowly surgeons and through the side of the hip. This is despite the fact that more damage to the muscles and cartilage ensues in this approach. In addition as this implant simply is a metal ball, sometimes with a plastic floating cup (bipolar version) which is literally 'pushed' into the acetabulum. It also brings in some cash from the Primary Care doctors for monitoring X-rays that have to be taken to check up on wear of the bony cup that is the acetabulum. It's almost beyond belief that anyone would consign a patient to receive a big metal ball 'stuffed' into a bone socket that's absolutely certain to wear away and cause pain in quite short order as it articulates with movement. Metal on bone; it doesn't take a scientist to work out which will wear first, especially in a younger, active patients, now does it? Alright, for the 85 year old with little in the way of exercise and a number of co-morbidity's, it may, just maybe justified after a fall, but as a first line treatment for most it's a cynical manipulation of guidelines and flies in the face of good practise and the welfare of the patient to reap the reward of the tariff.
Hip joints are one of the wonders of nature. They are a 'ball and socket' certainly, but one that has an interference fit that has a regenerative liner of cartilage and a fluid cushion that acts like the hydraulic fluid in a shock absorber, being 'squeezed' out and in as you walk and load the joint. As engineers we haven't even got close to this model nor are we ever likely to. There's no demand, well not from the medic's, the NHS and certainly not Big Pharma's devices wing. The patients, well we're the last people they care about, so long as the 'gravy train' keeps rolling. J and J's rubbish prosthesis is symptomatic of the 'device industry' and the final irony, as I keep hammering on about, is that most of these devices are implanted in women, because the female hip has much more 'articulation' than that of men to enable child birth, rendering their hips more liable to breakage. So women, often elderly women or those viewed as elderly by the NHS are the main recipients especially of 'hemi's', often when they and their peers see them as 'mature'. More misogyny, heavily tinged with ageism. Well there's a surprise!
You would think that in view of the large number of procedures undertaken in the NHS that the science would be driving the procedure, when in fact it is more custom and practise tinged heavily with vested interests and hubris. Orthopods (Orthopaedic Surgeon's) are generally viewed by Medicine, even other Surgeons as lacking in subtlety and intelligence. My view is somewhat more colourful and I view them as 'butchers' more than surgeons. Sure, it's a hard job, requiring physical strength and endurance, almost as much as skill because of the need to saw, hammer, drill and slice, with instruments more akin to a construction site and a butchers shop than an operating theatre. And the repair (or often not) of damaged hips epitomises this more than any other procedure. Dealing with hip trauma is probably the most difficult and dangerous procedure any surgeon undertakes. It is important then that the patient is paramount in the evaluation of which path to pursue as regards the protocol that is most efficacious.
It is not beyond my purview that many 'orthopods' are failed Rugby players, not that I attach any significance to that, except to say that their adherence to scientific evidence as a tenet of their professional conduct is perhaps somewhat lacking. It may sometimes be evident that their judgement of certain medical devices might be coloured by the presentation they last 'endured' in Barbados about the latest implantable device from one of the many makers of such engineering masterpieces (sic). One of these, of course is Depuy, a subsidiary of Johnson and Johnson (a family company). They make the 'Pinnacle' implant, which is a MOM (metal on metal) device using cobalt chrome, and this has been indicted as being subject to early failure. And more importantly, (I feel) of causing the migration into the bloodstream, bone and other tissues, of wear particles that are potentially life threatening in a number of ways.
The BMJ in conjunction with Newsnight undertook a study recently that highlighted this problem that is faced by a number of 'younger' patients who have been ill served by the installation of this design of prosthesis into their acetabulum. In truth the BMJ article is somewhat more comprehensive in it's condemnation of the device than was Paxman in the interview with the head 'honcho' of the MHRA who, it would seem had full knowledge of the 2010 recall by Depuy of it's ASR implant (Pinnacle) but seems to have done little about it. Nonetheless I did enjoy Paxman's taking Kent Wood's to task about the fundamentally supine attitude of his organisation when it comes to 'approving' medical devices, which essentially amounts to a review of the specification provided by the makers, because there are few if any clinical trials undertaken, except using the patient cohort as 'guinea pigs'.
As an engineer first and biologist second (but linking the two), I cannot understand how anyone would recommend the installation of any ball and socket device, in the human made from cobalt chrome that will be subject to metal on metal wear or indeed any frictional wear. The cobalt element of the material does have high strength, coupled with excellent corrosion resistance, but whilst it's salts are used by most animals especially ruminants, at high levels it can be toxic and it's compounds have been responsible for cardiomyopathy (heart muscle disease) in humans. Chromium is also quite toxic in its (VI) form except at very low levels and is a known carcinogen as well as being responsible for damage to the kidneys, liver and blood cells. Having said that, if this material had only been utilised for non-frictional component parts it is unlikely that there would have been a problem, but friction in metal to metal bearings throws off metal ions, eroding interfaces which increases gaps in mating surfaces thus introducing 'free play'. This is of course exponential, so the more wear the more the acceleration of that wear. The consequent contamination of the tissue surrounding the acetabulum and femoral stem and migration of these metal ions into the bloodstream promotes high levels of bone loss, cement collar erosion, cartilage damage, and many other toxic side effects that have yet to be fully evaluated.
When you introduce any 'foreign' body or substance into any living organism you have to be very sure that by so doing you are not making matters worse, but obviously this did not seem to impinge upon the corporate 'psyche' of J and J. Greed seems to have been the driving force and don't forget this company had last quarter earnings of $16.3 billion despite having to pay out $3 billion for the Pinnacle debacle in the US.
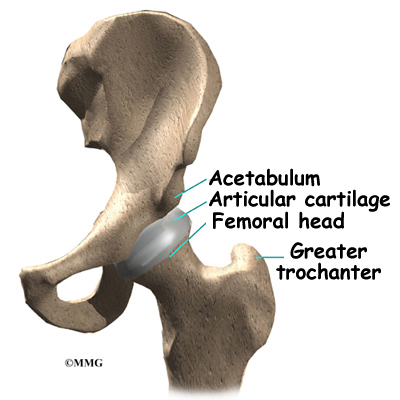 This design of implant was targeted at the younger audience and was sold as a 'low wear' prosthetic so as to avoid the need for revision surgery because this cohort tends to be physically very active. Activity promotes wear in any joint be it in humans' or in machinery, unless you can regularly lubricate that joint. There is some value in the concept of synovial fluid performing this function (the hip joints natural lubricant and hydraulic 'cushion'), but as this 'capsule' has effectively to be 'burst' during surgery for access, it is unlikely to function as it was designed by nature thereafter. The simple truth is that in our haste to address the increasing needs of an ageing and increasingly joint challenged society we have lost sight of many of the needs attendant upon the production of manufactured joints for implanting. And sadly it is not just in the metal to metal prosthetics that we have a problem.Many different materials have been tried over the years, especially plastics, sintered metals and ceramics. If one views success as being a bearing surface that does not wear out at all, and what wear does take place as being entirely benign, manufacturers have failed. Failed miserably in this context because all arthroplasty components have a finite life, so except in elderly patients, they are unlikely not to need revision at least once and in young patients possibly more.
This design of implant was targeted at the younger audience and was sold as a 'low wear' prosthetic so as to avoid the need for revision surgery because this cohort tends to be physically very active. Activity promotes wear in any joint be it in humans' or in machinery, unless you can regularly lubricate that joint. There is some value in the concept of synovial fluid performing this function (the hip joints natural lubricant and hydraulic 'cushion'), but as this 'capsule' has effectively to be 'burst' during surgery for access, it is unlikely to function as it was designed by nature thereafter. The simple truth is that in our haste to address the increasing needs of an ageing and increasingly joint challenged society we have lost sight of many of the needs attendant upon the production of manufactured joints for implanting. And sadly it is not just in the metal to metal prosthetics that we have a problem.Many different materials have been tried over the years, especially plastics, sintered metals and ceramics. If one views success as being a bearing surface that does not wear out at all, and what wear does take place as being entirely benign, manufacturers have failed. Failed miserably in this context because all arthroplasty components have a finite life, so except in elderly patients, they are unlikely not to need revision at least once and in young patients possibly more.UHMWPE has been the material of choice especially the newer 'crosslinked' varieties, for the manufacture of joint surfaces for some years now. Ultra high molecular weight polyethylene displays admirable self lubricating properties together little moisture absorption and considerable strength. But combinations of both this, ceramics and other metals have been tried, to come up with this goal of the perfect implant. None, including UHMWPE is devoid of particulate contamination of the tissue and blood of the recipient, although this last one is probably more benign than others. None are entirely so, and all wear is at a rate in proportion to the amount of use. So active people wear their implants out quicker.
As regards the NHS; well they invariably go for the cheapest they can get away with, THA (total hip arthroplasty) using cemented stems and UHMWPE bearing surfaces is usually the type most will get for either trauma repair or elective surgery, generally for osteoarthritis of the hip. Except for non-displaced or slightly displaced fractures, when the waters become extremely muddied. This is because of the payment system that prevails in trauma care which is based on a tariff for the most expensive treatment involved in a hospital 'stay', and the desire to keep the costs low, avoid re-admission and get rid of you as soon as possible. Trauma patients 'bugger up' the system, take up unplanned beds and play havoc with operating lists and theatre time allocations. If you aren't fixed quickly it costs more than the tariff. If they do something that's possibly short term, even if it's in your best interest as a patient, it's likely not to happen. If you are re-admitted for something that's a result of your initial admission, they won't get paid for it, so you are a burden.
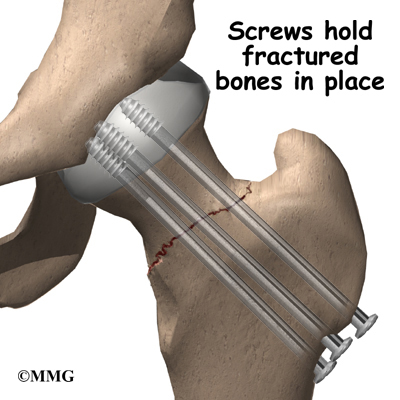 This has resulted on many occasions in the almost complete lack of hip repairs in trauma patients because of the incidence of failure. This is despite the fact that preservation of the native acetabulum and femoral head is the ideal solution. Failure rates of hip repairs are the subject of much conjecture but they are only about 25% in reasonably healthy people up to 65 or 70 years. They are also quick to do, much less traumatic, and can be undertaken, often without general anaesthetic, and sometimes without incision. Generally this requires nails or screws to fasten the joint together which are then left in place. If this fails, then you can go on to have a full procedure at a more leisurely pace and not as an emergency. But it won't happen, because if it fails, the Hospital involved will not get paid for the subsequent and much more expensive procedure to fix it because the 'system' attributes the blame to them. You will also have a longer recovery time as your leg will not be load bearing for some time, but you will be in possession of the best hip joint there is; your own! What you will likely receive for trauma, even if the fracture is so slightly displaced as to seem much like a 'crack', is the Hemiarthroplasty; the worst of all prostheses, because it's cheap, has a short operating window, and is likely to last five or six years, so they will be beyond the date whereby failure would not be paid for under the tariff.
This has resulted on many occasions in the almost complete lack of hip repairs in trauma patients because of the incidence of failure. This is despite the fact that preservation of the native acetabulum and femoral head is the ideal solution. Failure rates of hip repairs are the subject of much conjecture but they are only about 25% in reasonably healthy people up to 65 or 70 years. They are also quick to do, much less traumatic, and can be undertaken, often without general anaesthetic, and sometimes without incision. Generally this requires nails or screws to fasten the joint together which are then left in place. If this fails, then you can go on to have a full procedure at a more leisurely pace and not as an emergency. But it won't happen, because if it fails, the Hospital involved will not get paid for the subsequent and much more expensive procedure to fix it because the 'system' attributes the blame to them. You will also have a longer recovery time as your leg will not be load bearing for some time, but you will be in possession of the best hip joint there is; your own! What you will likely receive for trauma, even if the fracture is so slightly displaced as to seem much like a 'crack', is the Hemiarthroplasty; the worst of all prostheses, because it's cheap, has a short operating window, and is likely to last five or six years, so they will be beyond the date whereby failure would not be paid for under the tariff.The NHS likes this implant despite it's short life because it also has a lower dislocation rate, can be installed by relatively lowly surgeons and through the side of the hip. This is despite the fact that more damage to the muscles and cartilage ensues in this approach. In addition as this implant simply is a metal ball, sometimes with a plastic floating cup (bipolar version) which is literally 'pushed' into the acetabulum. It also brings in some cash from the Primary Care doctors for monitoring X-rays that have to be taken to check up on wear of the bony cup that is the acetabulum. It's almost beyond belief that anyone would consign a patient to receive a big metal ball 'stuffed' into a bone socket that's absolutely certain to wear away and cause pain in quite short order as it articulates with movement. Metal on bone; it doesn't take a scientist to work out which will wear first, especially in a younger, active patients, now does it? Alright, for the 85 year old with little in the way of exercise and a number of co-morbidity's, it may, just maybe justified after a fall, but as a first line treatment for most it's a cynical manipulation of guidelines and flies in the face of good practise and the welfare of the patient to reap the reward of the tariff.
Hip joints are one of the wonders of nature. They are a 'ball and socket' certainly, but one that has an interference fit that has a regenerative liner of cartilage and a fluid cushion that acts like the hydraulic fluid in a shock absorber, being 'squeezed' out and in as you walk and load the joint. As engineers we haven't even got close to this model nor are we ever likely to. There's no demand, well not from the medic's, the NHS and certainly not Big Pharma's devices wing. The patients, well we're the last people they care about, so long as the 'gravy train' keeps rolling. J and J's rubbish prosthesis is symptomatic of the 'device industry' and the final irony, as I keep hammering on about, is that most of these devices are implanted in women, because the female hip has much more 'articulation' than that of men to enable child birth, rendering their hips more liable to breakage. So women, often elderly women or those viewed as elderly by the NHS are the main recipients especially of 'hemi's', often when they and their peers see them as 'mature'. More misogyny, heavily tinged with ageism. Well there's a surprise!
Labels:
Arthroplasty,
Depuy,
Hemiarthroplasty,
Hip Fracture,
Hip Repair,
J and J,
Misogyny,
NHS,
Pinnacle
Subscribe to:
Comments (Atom)














